Rachel Lambert did not find brain health through theory. She found it through necessity. As the founder of Braincode Centers, Lambert now works at the forefront of neurofeedback and brain mapping, helping clients retrain their nervous systems for resilience, clarity, and longevity. But her path into this work was deeply personal.
On this episode of The Healthspan Collective podcast, Lambert shares how her own journey from chaos to regulation shaped a mission rooted in empowerment, adaptability, and long term mental wellbeing.
When the Brain Is Driving the Behavior
Growing up, Lambert sensed something was off long before she had language for it. “I was very reckless from a very young age,” she says. “I did a lot of drugs, a lot of alcohol.” Her impulsivity escalated to the point where her parents began asking a deceptively simple question, “Are you thinking before you’re acting?”
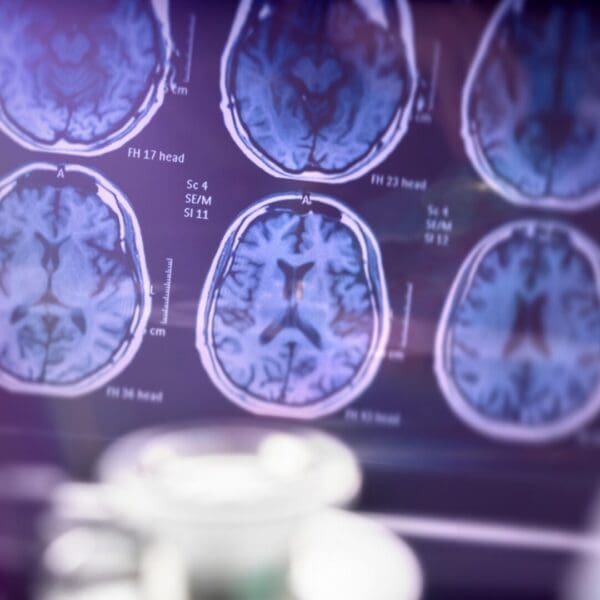
That question led her to a brain map. What it revealed changed everything. “My frontal cortex, which is like the decision maker of your brain, was going super super fast,” she explains. The pattern aligned with bipolar disorder, a diagnosis often framed as permanent. But neurofeedback offered another path. “At the end of it, I felt like for the first time ever I was in control of my brain,” she says. A follow up brain map showed “not one clinical pattern for bipolar.” At that moment, Lambert knew, “I want to do this for the rest of my life.”
Reading the Brain Without the Story
At Braincode Centers, the process begins with brain mapping, a quantitative EEG that reads brainwave activity. “It’s like an EKG of a heartbeat,” Lambert explains. The assessment does not rely on symptoms or emotional storytelling. “Thoughts are not going to dictate how your brainwaves function,” she says. Instead, the map reveals long standing neurological patterns that influence how a person operates.
This objectivity is key. “You don’t have to be anxious for us to see that your brain absolutely has a tendency to shift into a physiologically anxious place,” she explains. From anxiety and depression to ADHD, trauma, and cognitive decline, the brain tells its own story.
Neuroplasticity and the Art of State Shifting
Lambert describes neuroplasticity as adaptability. “If you can’t shift from a stressful day into being present with your family, that’s a lack of plasticity,” she says. Neurofeedback trains the brain to move between states more fluidly. “You have the ability to go the correct speed in the correct circumstances at the correct time.”
Through reward based training, the brain learns to self correct. “You’re not consciously thinking, okay brain do this,” she explains. “Your brain makes an auto correction much like learning how to ride a bike.” Over time, this repetition creates neurological permanency.
The ADHD Misunderstanding
One of the most eye opening insights Lambert shares is how misunderstood ADHD truly is. “Most people have the exact opposite pattern,” she says. Instead of a slow brain, many people’s brains are “going 150 miles per hour.” The symptoms may look the same, but the treatment is entirely different. “That’s why I’m always about actually measuring the very organ that’s creating symptoms.”
This individualized approach extends to motivation, focus, impulse control, and even cravings. Lambert recalls clients who suddenly lost interest in dessert. “We are not helping with weight loss,” she says. “We are helping with impulse control.”
Trauma, Addiction, and the Brain’s Memory
Lambert has worked extensively with addiction and trauma, including first responders and individuals recovering from substance use. “Even if you’re detoxed, you’re still going to have the same brain,” she explains. Neurofeedback helps rebalance brainwaves to support relapse prevention and regulation.
She is also candid about substances often perceived as benign. “If you are thinking utilizing THC on a regular basis is doing anything good for your brain, you are absolutely lying to yourself,” she says, noting clear patterns visible on brain maps.
Longevity Begins With Adaptability
When it comes to healthspan, Lambert emphasizes adaptability as a key predictor. “A huge predictor of longevity is how adaptive you are,” she says. Brain processing speed, particularly peak alpha, can signal early risk for dementia and cognitive decline. “You probably should want to know,” she says. “Because you can do a lot with that information.”
From children as young as six to adults in their nineties, Lambert reminds listeners that “the brain is always neuroplastic.”
Closing Reflection
Rachel Lambert’s work underscores a core truth of The Healthspan Collective, longevity is not about pushing harder, but about learning to shift, soften, and regulate. By teaching the brain how to adapt, rest, and respond, neurofeedback becomes a pathway not just to symptom relief, but to presence, resilience, and a longer, more connected life.
Listen to the full episode HERE!