A few weeks ago, during my usual early morning walk around 4:40 am, I slipped on wet ground while attempting to kick a tennis ball. The fall resulted in an anterior shoulder dislocation. My wife brought me to the emergency room, where my shoulder was reduced under IV propofol.
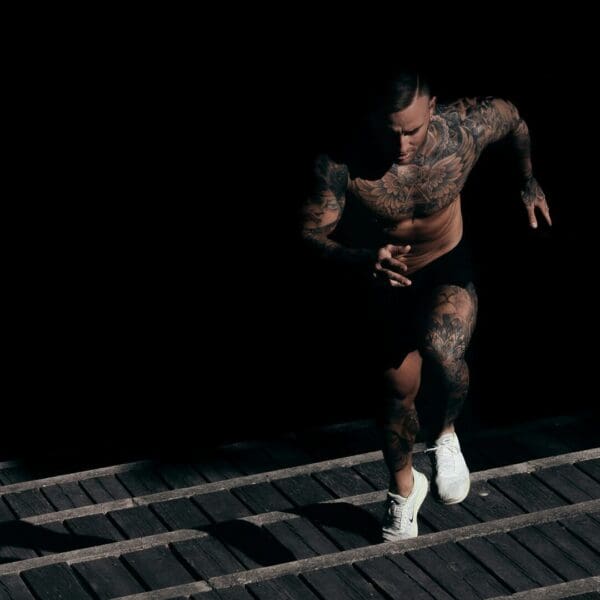
As an orthopedic surgeon by training, I was already familiar with the mechanics of shoulder dislocations and the movements to avoid during early recovery. The injury occurred over a long holiday weekend, and I was motivated to return to work as quickly and safely as possible. Rather than relying solely on standard rest and immobilization, I chose to apply a comprehensive regenerative protocol used at PUR-FORM to accelerate healing.
While I still do not have full strength, my recovery is progressing significantly faster than expected. I am already back to using the elliptical, working in my garden, and performing daily activities comfortably. The video above was recorded during this phase of recovery.
This article outlines the protocol I used and explains why it has been so effective.
Understanding Anterior Shoulder Dislocations
Anterior shoulder dislocations account for approximately 95 percent of all shoulder dislocations. In most cases, the humeral head is forced forward out of the joint, stretching or tearing the joint capsule, ligaments, rotator cuff muscles, and surrounding soft tissue.
Traditional recovery timelines are lengthy. Non surgical management often requires eight to twelve weeks before return to normal activity. Surgical stabilization may extend recovery to five or six months or longer.
Standard rehabilitation focuses primarily on restoring movement and strength. While this approach is important, it does not actively stimulate the biological processes that drive tissue repair at the cellular level.
Why Standard Recovery Often Feels Slow
A shoulder dislocation is more than a mechanical injury. It disrupts blood flow, damages microscopic tissue structures, and creates an inflammatory environment that can delay healing.
Typical rehabilitation progresses through phases of immobilization, gradual motion, and eventual strengthening. Even with excellent compliance, patients frequently experience persistent pain, stiffness, or incomplete recovery.
The missing piece is biological stimulation. Without addressing inflammation, circulation, cellular energy, and tissue remodeling, recovery depends largely on time rather than optimization.
A Multimodal Regenerative Approach to Healing
At PUR-FORM, we use a coordinated protocol that targets multiple stages of the healing process simultaneously. Each therapy supports a different aspect of tissue repair, creating a synergistic effect.
Phase One Clearing the Injury Environment
Systemic Enzymes Nattokinase and Serrapeptase
During the first few days after injury, systemic enzymes help clear inflammatory debris and excess fibrin from damaged tissue. Serrapeptase breaks down nonliving tissue and inflammatory byproducts, while nattokinase supports the body’s natural ability to dissolve abnormal fibrin.
This early cleanup is essential. A clear tissue environment allows growth factors and regenerative signals to reach the injury site more effectively.
Phase Two Powering Cellular Repair
Photobiomodulation Red and Infrared Light Therapy
Light therapy uses specific wavelengths of red and near infrared light to stimulate the mitochondria, the energy centers of cells. Repair cells require large amounts of energy to migrate, produce collagen, and rebuild damaged tissue.
Photobiomodulation increases cellular energy production while improving blood flow and reducing inflammation. This provides repair cells with the fuel they need to work efficiently and consistently.
Phase Three Improving Blood Flow and Delivery
Nitric Oxide Support With Neo 40
Nitric oxide is essential for healthy circulation. Neo 40 supports the body’s natural nitric oxide pathways, allowing blood vessels to relax and improve blood flow to injured tissue.
Adequate circulation ensures oxygen, nutrients, peptides, and growth signals can reach the shoulder. Nitric oxide also supports new blood vessel formation, which is critical during healing.
Phase Four Building New Blood Supply
BPC 157 Supporting Angiogenesis
BPC 157 is a peptide derived from a naturally occurring protective protein. It plays a key role in stimulating new capillary growth and improving microcirculation within injured tissue.
By promoting new blood vessel formation, BPC 157 helps restore oxygen and nutrient delivery directly to the healing shoulder. This is particularly important in joint injuries where blood flow is often compromised.
Phase Five Recruiting Repair Cells
TB 500 Mobilizing the Healing Response
TB 500 supports cell movement and repair cell recruitment. It enhances the ability of fibroblasts, immune cells, and progenitor cells to migrate quickly to the injury site.
Equally important, TB 500 helps regulate scar formation. By controlling excessive fibrotic activity, it promotes functional healing rather than stiff, restrictive scar tissue.
Phase Six Restoring Tissue Quality
GHK Cu Remodeling and Strengthening Tissue
GHK Cu is a naturally occurring copper peptide involved in tissue remodeling. It helps balance the breakdown of damaged collagen with the formation of new, organized collagen fibers.
The result is stronger, more flexible tissue that more closely resembles its original structure. This reduces stiffness, improves durability, and lowers the risk of reinjury.
How These Therapies Work Together
Each component of this protocol reinforces the others. Enzymes clear the environment. Light therapy provides energy. Nitric oxide improves circulation. BPC 157 builds blood supply. TB 500 brings in repair cells. GHK Cu ensures high quality tissue remodeling.
Rather than relying on time alone, this approach actively guides the body through each stage of healing.
Important Considerations and Patient Education
Some peptides discussed here are not FDA approved medications. Their use remains investigational and should only be considered under medical supervision. Safety data is limited, and sourcing through reputable compounding pharmacies is critical.
Results vary by individual. Age, baseline health, compliance, and participation in appropriate rehabilitation all influence outcomes.
This protocol is intended to complement standard medical care, not replace it. Proper diagnosis, reduction, immobilization, and physical therapy remain essential.
Conclusion
This multimodal regenerative protocol represents a modern approach to musculoskeletal injury recovery. By targeting the biological drivers of healing, it offers the potential to accelerate recovery while preserving tissue quality and function.
My own recovery from anterior shoulder dislocation supports the rationale behind this approach. While further clinical research is needed, the mechanisms are well supported and the early outcomes are compelling.
For patients and clinicians seeking advanced strategies to optimize recovery, this framework offers a thoughtful, physician guided path forward.
Dr. P